It is easy to dismiss healthcare software modernization as a “future project” when current systems appear stable. But stability isn’t the same as capability. Healthcare IT leaders know the drill. Every year, 80% of IT budget is poured into maintaining legacy systems that are outdated, slow, and resistant to change.
While the patches, workarounds, and performance tuning can help you buy time, they won’t help you make progress. Eventually, the costs of maintaining these legacy systems outweigh their benefits.
Hence, it is only by modernizing your healthcare software that you can remain competitive, enhance patient outcomes, and keep pace with evolving regulatory demands. Delaying this transition only widens the gap between current capabilities and demands of future healthcare delivery.
But where to start? And how to ensure that healthcare software modernization doesn’t become just another costly experiment? In this article, we’ll discuss viable ways to begin your modernization journey. But before that let’s understand why the path to modernization is often avoided.
Why is healthcare still clinging to legacy systems?
Healthcare leaders are aware of the inefficiencies of legacy software, but their hesitation to upgrade often boils down to four fears:
- Fear of downtime. (What if we disrupt critical operations during the transition?)
- Fear of data migration. (We’ve had decades of patient information. Can we move it without losing anything?)
- Fear of compliance. (Will modernization bring regulatory risks?)
- Fear of budget. (Healthcare software modernization costs money. How do we justify it?)
These fears are valid. But the cost of maintaining the status quo? Far greater.
Healthcare breaches cost organization an average of $9.77 million per incident, and 70% of these breaches occur at places still using outdated technology.
Then there is the impact on employee health. 81% of medical personnel, 77% of claims personnel, and 82% of clinical experts have personally suffered from burnout caused by poor software. Beyond being frustrating, it is fatiguing and negatively impacts those who are supposed to deliver optimal care.
Next is efficiency. According to Gartner, companies using outdated IT systems are 25% less productive than those using AI-based solutions. This disparity leads to slower response times, higher operating expenses, and, of course, a lot of frustrated employees.
And interoperability, let’s not forget. Legacy systems have a reputation for producing fragmented care and delayed diagnoses. And all of this adds up to poorer patient outcomes, such as higher readmission rates.
Lastly, there is the cost of opportunity. Healthcare organizations that stick with old technologies forgo the incredible advantages of AI-driven insights, effortless data sharing, and automated processes. These revolutionary technologies can dramatically enhance patient care and operational effectiveness, but they are simply unattainable if old technology is employed.
What does healthcare software modernization really mean?
Modernization isn’t a synonym for replacement.
It’s not about demolishing everything. Instead, it is all about upgrading and enhancing current software systems to get them more efficient, manageable, and scalable.
Modernization includes:
- Cloud migration. Transiting from on-premises servers to a scalable cloud infrastructure for higher flexibility and robustness.
- AI and machine learning integration. Powering clinicians with anomaly detection, predictive diagnosis, and individualized treatment recommendations.
- Interoperability improvements. Creating a smooth data flow through the implementation of contemporary integration platforms and FHIR APIs.
- Human-centered design. Streamlining clinician and patient workflows with intuitive, human-centered interfaces.
Healthcare software modernization is not a decision you make once; It’s a mindset shift. Some systems will need a gentle push towards the cloud. Others will demand a clean break. The real challenge is knowing the difference and having the resolve to act.
5 warning signs that scream “modernize your healthcare software now!”
If you are still unsure whether it’s time. Ask yourself these questions: –
- Do your clinicians have real-time access to a patient’s full medical history?
- Are your business decisions informed by predictive analytics?
- How many hours are lost due to manual data entry and error correction?
- Is your software architecture adaptable enough to changing legislation and technology?
- Could a cyberattack damage your system?
If those questions cause unease, your system is indicating its need for modernization.
Breaking down the healthcare software modernization journey
Successful healthcare software modernization is a multi-phased process that requires a clear plan. Here are the steps to guide the process: –
Thorough assessment
Start by carefully evaluating your current systems. Identify the problems, inefficiencies, and where outdated systems are holding development back. Involve stakeholders from administrative, clinical, and IT departments to fully understand the challenges. This step forms the basis for a sound modernization plan.
Set specific goals
What are your objectives for modernizing your healthcare software? Clear objectives are necessary, whether it’s to enhance data security, lower costs, or improve patient care. Well-defined goals ensure that the modernization supports your business plan and yields quantifiable outcomes.
Choose the right modernization approach
Select the modernization strategy most appropriate for your needs based on your evaluation and objectives.
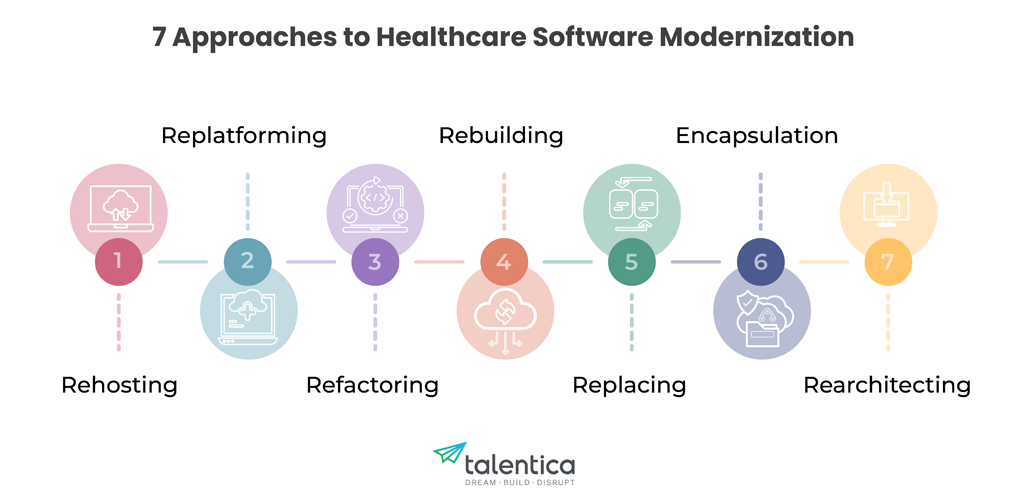
Rehosting
Rehosting is a popular approach that involves migrating current applications to a cloud platform. Without requiring significant code rewrites, this “lift and shift” technique can offer instant scalability and cost savings. It’s a smart first step when systems are stable, but infrastructure costs are spiraling.
Healthcare organizations under compliance stress tend to utilize rehosting to address uptime and disaster recovery needs. It is not a permanent solution, however. Without rethinking architecture, rehosting simply moves technical debt from one place to another. The systems remain inflexible, limiting innovation.
Benefits – Quick migration with minimal disruption. Idea for an organization that needs immediate cost savings or improved scalability.
Re-platforming
Re-platforming takes rehosting a step further. It is the process of making adjustments to current systems to better fit the cloud environment. Organizations can reduce maintenance costs and increase performance by tweaking the software to take advantage of cloud-native capabilities (scaling databases, automating backups, or enhancing security). This approach strikes a balance between adopting current efficiency and maintaining familiar functions.
It is particularly useful for improving electronic health record (EHR) systems that require uptime and rapid data access.
Benefits – Faster performance and reduced costs by using cloud-native features.
Refactoring
Refactoring is a commitment to untangle years of accumulated code. It’s for systems that work but creak under pressure. By cleaning up inefficiencies and rewriting parts of the application, organizations can eliminate performance bottlenecks and reduce operational costs. Refactoring requires a deep understanding of the system’s current design, even if it is less disruptive than a complete rebuild.
For example, predictive analytics solutions that require real-time data to support clinical decision-making often benefit from refactoring. The result? Clinicians will receive faster and more accurate information.
Benefits – Reduces technical debt, improves maintainability, and enables faster feature release.
Rebuilding
Some systems are beyond saving hence rebuilding it from scratch is sometimes the bravest choice. Rebuilding allows companies to create secure, scalable, and inherently contemporary systems. However, this strategy is resource-intensive and requires robust change management procedures and a clear objective. For healthcare CIOs, that’s terrifying, but so is maintaining a brittle system one patch at a time.
The upside? You get to rethink everything. Microservices instead of monoliths. Real-time analytics instead of delayed reports. AI-assisted diagnostics rather than static dashboards. For organizations building AI-powered diagnostics platforms or virtual care ecosystems, rebuilding is often the only way to meet the evolving demands.
Benefits– Frees organization from outdated technology constraints, enabling innovation and long-term resilience.
Replacing
When legacy systems no longer match up to modern healthcare needs, replacing them is the only sensible option. This process is similar to replatforming, but more complicated, since it involves building and integrating multiple, interconnected systems. New, custom-built platforms deliver sophisticated AI functionality, instant analytics, and effortless interoperability.
For health care organizations overwhelmed by regulatory complexity, contemporary, compliance-ready systems can ease the audit and reporting burden. For digital front doors (patient care portals that handle appointments, records, and virtual care), full replacement can transform the patient’s experience.
But replacement is disruptive. It demands clear communication, phased rollouts, and ongoing support. The best replacements happen when IT, clinical leadership, and patients are all engaged in the process.
Benefits- Opens the door for transformative innovation, often reducing long-term operational costs.
Encapsulation
Legacy healthcare systems often contain critical data and dismantling them without a strategy can be fatal. Encapsulation offers a way forward. Organizations can connect legacy systems with modern applications by wrapping them in APIs or service layers, reducing the risks associated with a complete replacement.
Telehealth systems, for example, frequently use encapsulation to access legacy EHR data. The end result is a seamless user experience that doesn’t reveal the underlying complexity.
However, encapsulation doesn’t offer a lasting solution. Even the best-encapsulated legacy systems will eventually need to be replaced.
Benefits– Enables interoperability, extends life of legacy systems, and reduces risk.
Rearchitecting
Rearchitecting is the solution to rigid, all-or-nothing systems. By using microservices, healthcare institutions can create adaptable and modular applications that adapt to changing business needs. Each service operates separately, from billing to medical information, streamlining and reducing the risk of upgrades and innovations.
For hospitals looking to increase their telehealth or remote monitoring capabilities, this is a major advantage. By being able to implement new services without completely redesigning the system, innovation can adapt to demand.
But technology isn’t the only aspect of re architecting. Changes in culture and governance are equally vital. Working together, cross-functional teams can ensure reliable systems and consistent data management.
Benefit- Improves scalability, resilience, and agility by breaking down monolithic systems.
So, which approach should you take?
The answer is rarely singular. Each of these approaches has advantages, and many organizations find that the best way to modernize healthcare software is to use a hybrid approach.
Incorporate new technologies
Modern technologies are revolutionizing healthcare, from digital twins for patient modeling to AI-based diagnostics. Consider integrating:
- AI and machine learning: For individualized treatments and prognoses.
- Cloud computing: For remote access and scalability.
- Blockchain: For secure and impenetrable data management.
- Wearable devices and IoT: For instant patient monitoring.
Select technology based on your goals, not just what’s popular.
Phased implementation
Rather than implementing modernization all at once, do it in phases. By implementing this phased strategy, you can test and improve each component before a full implementation, thus minimizing disruptions to normal operations. Prioritize critical systems before progressively expanding to other domains.
Ongoing training and support
User adoption is essential for healthcare software modernization. All employees, including frontline clinical and IT staff, should receive extensive training. Regular updates and ongoing support will help ensure new systems are used efficiently and that any issues are resolved promptly.
Measure and optimize
How will you know if modernization is paying off? Once the new systems are operational, monitor performance against established goals. To assess progress, use key performance indicators (KPIs) such as reduced wait times, improved patient outcomes, and cost savings. Use the information to optimize procedures and drive further progress.
| KPI Category | KPI Metric | Measurement Method | Significance |
|---|---|---|---|
| Patient Experience | Average Patient Wait Time (Check-in to Care) | System reports, patient surveys, manual time tracking | Reduced wait times indicate improved efficiency and patient satisfaction. |
| Patient Satisfaction Scores (CSAT/NPS) | Patient surveys (online, in-person), feedback forms | High scores reflect positive patient experiences with digital services and care delivery. | |
| Telehealth Adoption Rate | System reports, patient portal usage data | Measures the effectiveness of telehealth initiatives and patient engagement with remote care. | |
| Clinical Outcomes | Readmission Rates | EHR/EMR data analysis, hospital records | Lower readmission rates indicate improved care coordination and patient management. |
| Time to Diagnosis | System reports, time tracking of diagnostic procedures | Shorter diagnosis times mean faster treatment and potentially better patient outcomes. | |
| Improved Chronic Disease Management Metrics | EHR/EMR data, patient monitoring data, lab results | Measures improvements in managing chronic conditions through proactive care and remote monitoring. (e.g. A1C levels, blood pressure control) | |
| Operational Efficiency | Reduction in Administrative Costs | Financial reports, cost analysis of administrative tasks | Cost savings demonstrate the impact of automation and streamlined workflows. |
| Data Interoperability Rate | System reports, tracking of successful data exchanges between systems | Indicates the effectiveness of data sharing initiatives and improved care coordination. | |
| System Uptime | System monitoring tools, IT support logs | High uptime ensures consistent access to critical systems and minimizes disruptions. | |
| Regulatory Compliance | Reduction in Compliance Penalties | Financial records, audit reports | Fewer penalties indicate improved adherence to regulations (HIPAA, etc.). |
| Data Security Incident Rate | Security incident logs, audit reports, system security reports | Low incident rates demonstrate the effectiveness of cybersecurity measures. | |
Financial Performance | Return on Investment (ROI) of Modernization | Financial analysis comparing costs of modernization with benefits (cost savings, increased revenue) | Shows the overall value and financial impact of the modernization investment. |
Collaborate with technology partners
Collaborating with experienced technology providers can have a significant impact. Look for partners with a track record of successful implementations and deep knowledge of the healthcare industry. Working together ensures you have access to the latest advancements and expert advice throughout the healthcare software modernization process.
What does success look like?
A successful healthcare software modernization project will:
- Optimize processes to reduce operating expenses.
- Improve patient outcomes by providing real-time information.
- Provide medical professionals with AI-based decision-making support.
- Automated monitoring can help ensure regulatory compliance.
- Easily scale to adapt to future needs.
Most importantly, it will turn technology into an asset rather than a hindrance.
Overcoming the challenges of healthcare software modernization
While modernizing healthcare software offers many benefits, the journey is not without its challenges. Below are some common obstacles and solutions:
Integration with legacy systems
Integrating new and existing software with older systems can be difficult. Many healthcare organizations struggle to reconcile outdated interfaces and diverse data types. Bridging the gap between legacy and new systems using middleware and APIs is a popular way to phase out legacy components while maintaining data continuity.
Data quality and migration
There are several obstacles to overcome when migrating large volumes of patient data from outdated systems to modern platforms. Thorough preparation and the use of specialized data migration tools are required to ensure data security, accuracy, and integrity during the migration. Implementing data governance frameworks and conducting regular data quality audits are essential for success.
Resistance to change
Healthcare professionals often resist new systems because they are accustomed to old ones. To combat this, organizations need to invest in comprehensive training programs, involve end users from the beginning of the process, and demonstrate the true benefits of modernization. Creating a culture that embraces change is as important as the technology itself.
Upfront costs and ROI concerns
The cost of modernization projects can be high, and the return on investment (ROI) may not materialize immediately. On the other hand, long-term benefits—such as lower administrative overhead, improved patient outcomes, and increased operational efficiency—often outweigh the initial costs. It’s critical to create a phased implementation strategy that spreads expenses over time and consistently demonstrates benefits through quantifiable KPIs.
Compliance and cybersecurity
The importance of cybersecurity is crucial given the growing threat of cyberattacks. Modern healthcare software must meet robust security standards and regulatory criteria. Investing in cutting-edge cybersecurity solutions like confidential computing helps increase patient and regulatory confidence while protecting patient data. Continuous updates, frequent audits, and proactive monitoring are crucial elements of a modernized system.
Even Pankaj Mendki, our head of Emerging Technology, highlights the value of confidential computing. According to him, this technology can help healthcare companies protect patient data at every stage of its lifecycle, strengthening conventional encryption and protecting private data during processing.
Conclusion
Healthcare software modernization is about moving forward and not just catching up. It’s about ensuring that the patient has a seamless experience, that their data is secure, and that they receive individualized treatment the next time they enter the hospital.
Perhaps most important is empowering those who provide medical care.
Ready to take the next step in your healthcare software modernization journey? Let’s have a conversation then.

 " class="img-responsive width-100 featured-img mar-b-5" loading="lazy" />
" class="img-responsive width-100 featured-img mar-b-5" loading="lazy" />







